What to expect
The peritonectomy surgeons and experienced team of doctors will see you every morning 7 days a week including weekends and public holidays. During the day the team will see you as needed and will do a ward round again in the afternoon. You may wish to ask questions at these times so we suggest it is a good idea to have a family member present or advise you to write your questions in advance, so you don’t forget them.
When you are being discharged we will organise follow-up appointments with the team doctors, if required, in the ambulatory care unit where they may review your bloods or remaining wounds etc.
You will be given an appointment to see your surgical consultant in the rooms a few weeks after discharge and we will ensure you have a follow up appointment with the medical oncologist if it is required.
If you have any of the following ongoing or new symptoms after discharge you will need to call us asap:
- temperature
- pain
- nausea or vomiting
- shortness of breath
- wound redness or oozing
Contact the Peritonectomy CNC during office hours (02) 9113 1111, pager 279 or if after hours contact the surgical team via the emergency number 0427 748 485.
What a patient will look like after surgery
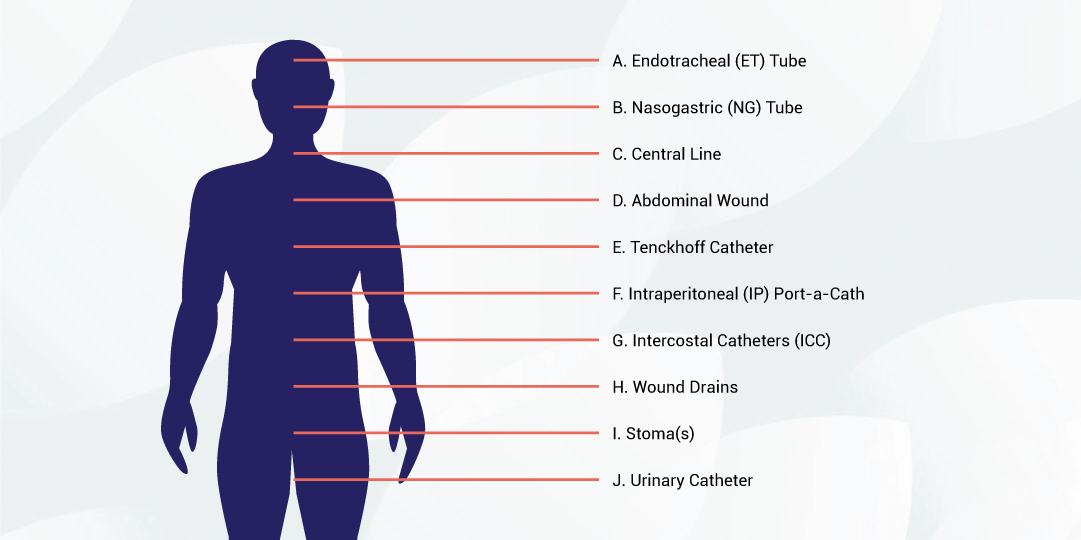
A – Endotracheal (ET) Tube
Located in your mouth and throat, this tube is connected to the ventilator to help you breathe.
B – Nasogastric (NG) Tube
Located in your nose and going down into your stomach, this tube drains your stomach contents until your bowel starts functioning again.
C – Central Line
Usually located in your neck, this is an intravenous line that is inserted into a large vein leading to your heart prior to surgery. The purpose of this line is to provide long-term venous access for administering fluids, medications, blood products and nutrition.
D – Abdominal Wound
This will usually extend from the sternum to the pubis.
E – Tenckhoff Catheter
This is a soft thin tube placed during surgery through which post-operative chemotherapy is given into the abdominal cavity.
E: Intraperitoneal (IP) Port-a-Cath ®
This is a small plastic device that is implanted below the ribcage. It is accessed externally with a special needle and is used to administer the post-operative chemotherapy into the abdominal cavity (See page 8).
F – Intercostal Catheters (ICC)
These are drains placed through the skin and into the chest cavity. They are used to drain fluid and air from the area around your lungs.
G – Wound Drains
Exiting your belly, these are large bore drains that are placed for the purpose of draining blood, body fluid and chemotherapy out of your abdomen.
H – Stoma/s
If the bowel cannot be safely joined back together, it may need to be brought to the surface as a stoma (colostomy/ileostomy) with bowel contents draining into a bag. Stomas may be temporary or permanent depending on the amount of bowel removed and other circumstances.
I – Urinary Catheter
A tube that drains urine from the bladder. This may also be used to measure the pressure in your abdomen.
What can be done to maximise the chance of success?
Keeping active, exercise daily e.g. walking, eating as healthily as possible and having a healthy attitude are the things you can do to help cope with the treatment and maximise your chance of success. It is important that you ask any questions that are on your mind.
If you are a smoker it is advised that you cease as soon as possible. There is clear evidence that smoking, apart from affecting your lungs and increasing the risk of chest infection post surgery, can also have a detrimental effect on healing, leading to wound breakdown and fistula. We acknowledge it may be difficult to stop and advise you consult with your GP for guidance.
We have a team of people to look after your surgery, anaesthesia, chemotherapy, intensive care stay and recovery time on the ward. Our job is to make sure everything goes as well as possible for you. The extensive testing you have and the appointments with many team members are all to make sure that this surgery and chemotherapy are likely to be beneficial for you and that any risks are minimised. For example, it is important to correct anaemia and/or iron deficiency prior to surgery, this will help to reduce the amount of blood transfusions required during your operation. There is evidence to suggest that blood transfusions can increase the risk of complications and overall survival post-surgery. We may ask you see your GP to arrange an iron infusion while you are preparing for your surgery.
What happens if treatment is not successful?
Before you undergo the operation, we do need to address the possibility that things might not go well and that major complications could occur. It can be difficult if this happens in ICU because you may well be sedated and unable to discuss this at the time.
St George Peritonectomy unit’s mortality rate for this procedure is 1.5%-2%. Although the likelihood of major life-threatening complications is very low, it is devastating when it happens and therefore extremely important that you are prepared for this possibility in advance. It is a good idea to have discussed with your family or friends what your wishes would be in the event you were faced with significant disability or a minimal chance of recovery. Indeed, it is often a good idea to decide in advance who you would like the doctors to talk to if they are not able to talk to you about your treatment and care, and then to give that person some indication of what your wishes would likely be. You can help that person by telling them what would be important to you. This can be formally documented in an ‘Advance Care Directive’ please ask your treating team for further information if required.