For Patients
It has been suggested to you that you consider undergoing a treatment program involving both surgery and intraperitoneal chemotherapy because you have a cancer which involves the peritoneal cavity.
This surgery in combination with intraperitoneal chemotherapy is a standard treatment which may be considered for the following conditions: pseudmyxoma peritonei, appendix cancer, colorectal cancer, ovarian cancer, peritoneal mesothelioma and small bowel cancer.
It may be considered for some other rare cancers as a non-standard but potentially therapeutic treatment.
The decision about whether to accept an offer of treatment may be a difficult one for you and we want to help you make a good decision in your particular circumstance. We hope that the information contained here will be useful to you in your discussions with your doctors and your family. We encourage you to seek their help and advice.
You can expect your doctors to explain your condition, treatment options and intent, prognosis (with and without treatment) as well as any risks associated with the proposed treatment in an accurate, clear and sensitive manner.
The purpose of this information is to advise you of these matters, and to assist you in your decision-making. You have the right to refuse any test or treatment proposed by your doctors. They will carefully evaluate any request you make for treatment and, if they think your request for a test or treatment is inadvisable, they will explain to you why they cannot comply with your request. If possible, they will offer you the opportunity of a second opinion.
We encourage you to discuss the information in this contained here and through the St George Peritonectomy website with anyone you feel would be helpful. This person may be a family member, your GP or your referring doctor. The treatment and the issues involved are very complicated. If there is anything you don’t understand, please let us know.

What is the peritoneal cavity?
The peritoneum is a thin lining that wraps around the bowel and other organs in your abdomen, similar to the skin around a sausage. It also lines the inside of the abdomen wall. A double fold of the peritoneum forms the fatty apron (called the omentum) that hangs over your bowel inside the abdominal cavity.
When the abdomen is opened surgically, the space between all the loops of bowel, the lining of the belly wall and the omentum is called the peritoneal cavity.
What is Peritoneal Cancer Index (PCI)?
You will hear us refer to Peritoneal Cancer Index (PCI). The PCI is the measuring tool we use to determine the volume and spread of disease (peritoneal carcinomatosis or metastasis) within your peritoneal cavity. The PCI thus can indicate or determine the treatment options that may be of benefit to you.
The abdomen is divided into 13 sections (pictured above). To estimate the PCI, the largest cancer growth in each section is given a score between 0-3 based on its size. The PCI is the total of all these scores. Since there are 13 sections, the maximum score is 39. In most instances the lower your PCI, the more likely surgery is going to be beneficial for you.
Radiological studies help us to determine the amount of disease present before you are operated on (‘preoperatively’). Sometimes to determine PCI we may also perform a laparoscopy (which is a look into the abdominal cavity with a thin telescope) to better assess amount of cancer. The PCI is important for determining the suitability of surgery for some cancers such as colon cancer (i.e. if the PCI is greater than 15 then peritonectomy is not beneficial). For other conditions like pseudmyxoma, PCI is used to determine the urgency of surgery.
During your surgery the PCI score will be formally assessed. It is quite common for the volume of disease to be higher on that day than was your pre-operative score. As a result, sometimes the proposed surgical procedure may not be able to continue as planned. For some cancers the PCI at the time of surgery can help determine the prognosis after surgery.
What is a Peritonectomy?
Surgery to remove cancer from the peritoneal cavity is known as peritonectomy or cytoreductive surgery (meaning surgical removal of all visible cancer nodules with curative intent). In our unit the peritonectomy procedure normally incorporates heated intraperitoneal chemotherapy (HIPEC), at time of surgery, with or without early post-operative peritoneal chemotherapy (EPIC).
Peritonectomy
This procedure is the complete removal of all visible tumour from the peritoneal cavity. The amount of surgery required to achieve this varies a lot between people depending on the extent of the disease and PCI. It is not possible to predict exactly how much surgery will be required to remove all the tumour. Variable from an 8-12 hours procedure, surgery is followed by treating the surface of the abdominal cavity with heated intraperitoneal chemotherapy.
It is not uncommon that there is a need to remove some of the bowel as a part of this procedure. If the bowel cannot be safely joined back together, it may need to be brought to the surface as a stoma (colostomy/ileostomy) with bowel contents draining into a bag. Stomas may be temporary or permanent depending on the amount of bowel removed and other circumstances. Other organs which may need to be removed, if involved by cancer, include your gall bladder, spleen, stomach, kidney as well as the female reproductive organs (including uterus, ovaries and fallopian tubes). Most normal activity will be able to continue without these organs. In your situation any likely effect on your daily life will be explained to you. The ability to have children may be significantly altered following removal of any reproductive organs.
Post-surgery, many of the possible difficulties/complications arise from your body having to cope with such a large operation. However, the Peritonectomy team will be able detect and look after these complications. The more extensive the surgery, the more time may be needed in the intensive care and in the hospital after the operation.
Hot Chemotherapy (HIPEC) – Heated intra-peritoneal chemotherapy
Once all visible tumour has been removed, a chemotherapy drug is given directly into your belly (the ‘peritoneal cavity’) whilst it is still open. This is a major treatment advantage as it allows us to put the chemotherapy directly into the area where the cancer cells are. We also heat the chemotherapy to around 40 degrees Celsius, which increases the effectiveness of the chemotherapy. After 30 to 90 minutes (depending on which drug is used) the chemotherapy is removed, everything is sewn back up and you will then be taken directly to the Intensive Care Unit (ICU) without being woken up.
The type of chemotherapy used depends on the type of cancer you have.
If we are unable to achieve complete removal of the cancer, or if we determine at the time of surgery there is a high risk of chemotherapy complications, we may omit the HIPEC and change the treatment plan from curative to palliative intent.
HIPEC is sometimes given by key-hole surgery (called ‘laparoscopy’) to control fluid build- up (called ‘ascites’) inside the abdomen from the cancer. In this instance the cancer is not removed. This is a palliative procedure.
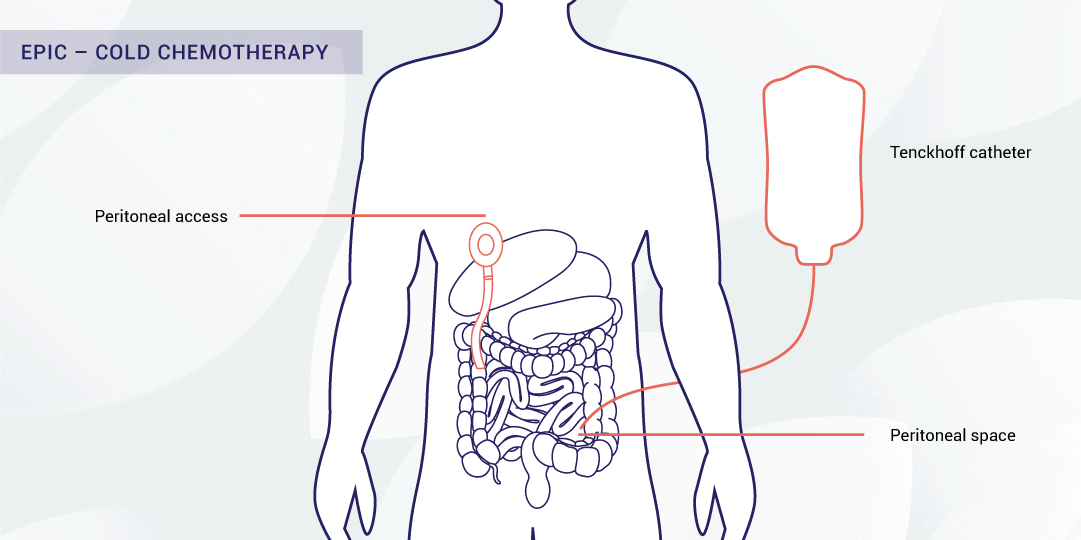
Cold Chemotherapy (EPIC) – Early post-operative intraperitoneal chemotherapy
While you are in ICU, we aim to start the third phase of the treatment the day after your operation. Further chemotherapy with a drug called 5FU (5-Fluorouracil) is given directly into the peritoneal cavity through a thin tube called a Tenckhoff Catheter® or very occasionally through a device called a Port-a-Cath®, which will be inserted into the peritoneal cavity at the time of the operation for this purpose. This is usually used for pseudmyxoma peritonei and occasionally for colorectal and appendix cancer.
Once EPIC is completed, the Tenckhoff Catheter® is removed at the bed side. If a Port-a-Cath® has been used (less common) it is removed as a minor surgical procedure, usually prior to discharge from hospital.
A one litre test bag of fluid (not chemotherapy) is run into the belly first to check that there are no leaks from wounds or drain sites. This fluid is later drained out via the abdominal drains. Provided this is successful, a further litre bag of fluid containing the chemotherapy will then be run into the belly, where it will remain for approximately 23 hours. We would normally aim to repeat this treatment every day for a total of up to 5 days. This EPIC will allow maximum exposure and efficacy of chemotherapy to cancer cells with fewer side effects comparing to systemic chemotherapy
Please note that sometimes there is a need for us to modify this plan based on how things have gone in the operation and in ICU, as well as how your body has responded to the operation. You can be assured that we will take every care to make sure that the surgery is appropriate for your particular condition.
Do not hesitate to ask us any questions about the chemotherapy plan after the operation.